Latest News,Articles and Events
Prostate cancer is the development of cancer in the prostate, a gland in the male reproductive system. Most prostate cancers are slow growing; however, some grow relatively quickly. The cancer cells may spread from the prostate to other area of the body, particularly the bones and lymph nodes. It may initially cause no symptoms. In later stages, it can lead to difficulty urinating, blood in the urine or pain in the pelvis, back, or when urinating. A disease known as benign prostatic hyperplasia may produce similar symptoms. Other late symptoms may include feeling tired due to low levels of red blood cells.
Factors that increase the risk of prostate cancer include older age, a family history of the disease, and race. About 99% of cases occur in males over the age of 50. Having a first-degree relative with the disease increases the risk two to threefold. In the United States, it is more common in the African American population than the White American population. Other factors that may be involved include a diet high in processed meat, red meat or milk products or low in certain vegetables. An association with gonorrhea has been found, but a reason for this relationship has not been identified. An increased risk is associated with the BRCA mutations. Prostate cancer is diagnosed by biopsy. Medical imaging may then be done to determine if the cancer has spread to other parts of the body.
Prostate cancer screening is controversial. Prostate-specific antigen (PSA) testing increases cancer detection, but it is controversial regarding whether it improves outcomes. Informed decision making is recommended when it comes to screening among those 55 to 69 years old. Testing, if carried out, is more reasonable in those with a longer life expectancy. While 5α-reductase inhibitors appear to decrease low-grade cancer risk, they do not affect high-grade cancer risk and thus are not recommended for prevention. Supplementation with vitamins or minerals does not appear to affect the risk.
Many cases are managed with active surveillance or watchful waiting. Other treatments may include a combination of surgery, radiation therapy, hormone therapy or chemotherapy. When it only occurs inside the prostate, it may be curable. In those in whom the disease has spread to the bones, pain medications, bisphosphonates and targeted therapy, among others, may be useful. Outcomes depend on a person's age and other health problems as well as how aggressive and extensive the cancer is. Most people with prostate cancer do not end up dying from the disease. The 5-year survival rate in the United States is 99%. Globally, it is the second most common type of cancer and the fifth leading cause of cancer-related death in men. In 2012, it occurred in 1.1 million men and caused 307,000 deaths. It was the most common cancer in males in 84 countries, occurring more commonly in the developed world. Rates have been increasing in the developing world. Detection increased significantly in the 1980s and 1990s in many areas due to increased PSA testing. Studies of males who died from unrelated causes have found prostate cancer in 30% to 70% of those over age 60.
Prostate cancer is associated with urinary dysfunction as the prostate gland surrounds the prostatic urethra. Changes within the gland, therefore, directly affect urinary function. Because the vas deferens deposits seminal fluid into the prostatic urethra, and secretions from the prostate gland itself are included in semen content, prostate cancer may also cause problems with sexual function and performance, such as difficulty achieving erection or painful ejaculation.
Metastatic prostate cancer that has spread to other parts of the body can cause additional symptoms. The most common symptom is bone pain, often in the vertebrae (bones of the spine), pelvis, or ribs. Spread of cancer into other bones such as the femur is usually to the proximal or nearby part of the bone. Prostate cancer in the spine can also compress the spinal cord, causing tingling, leg weakness and urinary and fecal incontinence.
There are also several other tests that can be used to gather more information about the prostate and the urinary tract. Digital rectal examination (DRE) may allow a doctor to detect prostate abnormalities. Cystoscopy shows the urinary tract from inside the bladder, using a thin, flexible camera tube inserted down the urethra. Transrectal ultrasonography creates a picture of the prostate using sound waves from a probe in the rectum. But the only test that can fully confirm the diagnosis of prostate cancer is a biopsy, the removal of small pieces of the prostate for microscopic examination.
Prostate MRI has better soft tissue resolution than ultrasound.
MRI in those who are at low risk might help people choose active surveillance, in those who are at intermediate risk it may help with determining the stage of disease, while in those who are at high risk it might help find bone disease.
Currently (2011), MRI is used to identify targets for prostate biopsy using fusion MRI with ultrasound (US) or MRI-guidance alone. In men who are candidates for active surveillance, fusion MR/US guided prostate biopsy detected 33% of cancers compared to 7% with standard ultrasound guided biopsy.
Prostate MRI is also used for surgical planning for men undergoing robotic prostatectomy. It has also shown to help surgeons decide whether to resect or spare the neurovascular bundle, determine return to urinary continence, and help assess surgical difficulty.
For Prostate MRI exists the PI-RADS Reporting system. PI-RADS is an acronym for Prostate Imaging-Reporting and Data System, defining standards of high-quality clinical service for multi-parametric Magnetic Resonance Imaging (mpMRI), including image creation and reporting.
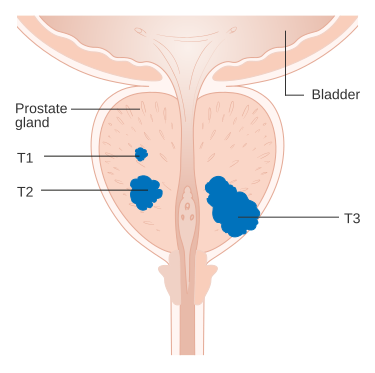
The most important distinction made by any staging system is whether or not the cancer is still confined to the prostate. In the TNM system, clinical T1 and T2 cancers are found only in the prostate, while T3 and T4 cancers have spread elsewhere. Several tests can be used to look for evidence of spread. Medical specialty professional organizations recommend against the use of PET scans, CT scans, or bone scans when a physician stages early prostate cancer with low risk for metastasis. Those tests would be appropriate in such cases as when a CT scan evaluates spread within the pelvis, a bone scan look for spread to the bones, and endorectal coil magnetic resonance imaging to closely evaluate the prostatic capsule and the seminal vesicles. Bone scans should reveal osteoblastic appearance due to increased bone density in the areas of bone metastasis—opposite to what is found in many other cancers that metastasize.
After a prostate biopsy, a pathologist looks at the samples under a microscope. If cancer is present, the pathologist reports the grade of the tumor. The grade tells how much the tumor tissue differs from normal prostate tissue and suggests how fast the tumor is likely to grow. The Gleason system is used to grade prostate tumors from 2 to 10, where a Gleason score of 10 indicates the most abnormalities. The pathologist assigns a number from 1 to 5 for the most common pattern observed under the microscope, then does the same for the second-most-common pattern. The sum of these two numbers is the Gleason score.
The data on the relationship between diet and prostate cancer is poor. In light of this the rate of prostate cancer is linked to the consumption of the Western diet.There is little if any evidence to support an association between trans fat, saturated fat, and carbohydrate intake and risk of prostate cancer.Evidence regarding the role of omega-3 fatty acids in preventing prostate cancer does not suggest that they reduce the risk of prostate cancer, although additional research is needed.Vitamin supplements appear to have no effect and some may increase the risk.High calcium intake has been linked to advanced prostate cancer.[83] Consuming fish may lower prostate cancer deaths but does not appear to affect its occurrence.Some evidence supports lower rates of prostate cancer with a vegetarian diet.There is some tentative evidence for foods containing lycopene and selenium.Diets rich in cruciferous vegetables, soy, beans and other legumes may be associated with a lower risk of prostate cancer, especially more advanced cancers.
Men who get regular exercise may have a slightly lower risk, especially vigorous activity and the risk of advanced prostate cancer.
 |
| By Cancer Research UK - Original email from CRUK, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=34333915 |
Factors that increase the risk of prostate cancer include older age, a family history of the disease, and race. About 99% of cases occur in males over the age of 50. Having a first-degree relative with the disease increases the risk two to threefold. In the United States, it is more common in the African American population than the White American population. Other factors that may be involved include a diet high in processed meat, red meat or milk products or low in certain vegetables. An association with gonorrhea has been found, but a reason for this relationship has not been identified. An increased risk is associated with the BRCA mutations. Prostate cancer is diagnosed by biopsy. Medical imaging may then be done to determine if the cancer has spread to other parts of the body.
Prostate cancer screening is controversial. Prostate-specific antigen (PSA) testing increases cancer detection, but it is controversial regarding whether it improves outcomes. Informed decision making is recommended when it comes to screening among those 55 to 69 years old. Testing, if carried out, is more reasonable in those with a longer life expectancy. While 5α-reductase inhibitors appear to decrease low-grade cancer risk, they do not affect high-grade cancer risk and thus are not recommended for prevention. Supplementation with vitamins or minerals does not appear to affect the risk.
Many cases are managed with active surveillance or watchful waiting. Other treatments may include a combination of surgery, radiation therapy, hormone therapy or chemotherapy. When it only occurs inside the prostate, it may be curable. In those in whom the disease has spread to the bones, pain medications, bisphosphonates and targeted therapy, among others, may be useful. Outcomes depend on a person's age and other health problems as well as how aggressive and extensive the cancer is. Most people with prostate cancer do not end up dying from the disease. The 5-year survival rate in the United States is 99%. Globally, it is the second most common type of cancer and the fifth leading cause of cancer-related death in men. In 2012, it occurred in 1.1 million men and caused 307,000 deaths. It was the most common cancer in males in 84 countries, occurring more commonly in the developed world. Rates have been increasing in the developing world. Detection increased significantly in the 1980s and 1990s in many areas due to increased PSA testing. Studies of males who died from unrelated causes have found prostate cancer in 30% to 70% of those over age 60.
Signs and symptoms
Early prostate cancer usually has no clear symptoms. Sometimes prostate cancer does cause symptoms, often similar to those of diseases such as benign prostatic hyperplasia. These include frequent urination, nocturia (increased urination at night), difficulty starting and maintaining a steady stream of urine, hematuria (blood in the urine), and dysuria (painful urination). A study based on the 1998 Patient Care Evaluation in the US found that about a third of patients diagnosed with prostate cancer had one or more such symptoms, while two-thirds had no symptoms.Prostate cancer is associated with urinary dysfunction as the prostate gland surrounds the prostatic urethra. Changes within the gland, therefore, directly affect urinary function. Because the vas deferens deposits seminal fluid into the prostatic urethra, and secretions from the prostate gland itself are included in semen content, prostate cancer may also cause problems with sexual function and performance, such as difficulty achieving erection or painful ejaculation.
Metastatic prostate cancer that has spread to other parts of the body can cause additional symptoms. The most common symptom is bone pain, often in the vertebrae (bones of the spine), pelvis, or ribs. Spread of cancer into other bones such as the femur is usually to the proximal or nearby part of the bone. Prostate cancer in the spine can also compress the spinal cord, causing tingling, leg weakness and urinary and fecal incontinence.
Diagnosis
The American Cancer Society's position regarding early detection by PSA testing is "Research has not yet proven that the potential benefits of testing outweigh the harms of testing and treatment. The American Cancer Society believes that men should not be tested without learning about what we know and don’t know about the risks and possible benefits of testing and treatment. Starting at age 50, (45 if African American or brother or father suffered from condition before age 65) talk to your doctor about the pros and cons of testing so you can decide if testing is the right choice for you."There are also several other tests that can be used to gather more information about the prostate and the urinary tract. Digital rectal examination (DRE) may allow a doctor to detect prostate abnormalities. Cystoscopy shows the urinary tract from inside the bladder, using a thin, flexible camera tube inserted down the urethra. Transrectal ultrasonography creates a picture of the prostate using sound waves from a probe in the rectum. But the only test that can fully confirm the diagnosis of prostate cancer is a biopsy, the removal of small pieces of the prostate for microscopic examination.
Prostate imaging
Ultrasound (US) and magnetic resonance imaging (MRI) are the two main imaging methods used for prostate cancer detection. Urologists use transrectal ultrasound during prostate biopsy and can sometimes see a hypoechoic area (tissues or structures that reflect relatively less of the ultrasound waves directed at them). As ultrasound has poor tissue resolution, it is generally not used clinically.Prostate MRI has better soft tissue resolution than ultrasound.
MRI in those who are at low risk might help people choose active surveillance, in those who are at intermediate risk it may help with determining the stage of disease, while in those who are at high risk it might help find bone disease.
Currently (2011), MRI is used to identify targets for prostate biopsy using fusion MRI with ultrasound (US) or MRI-guidance alone. In men who are candidates for active surveillance, fusion MR/US guided prostate biopsy detected 33% of cancers compared to 7% with standard ultrasound guided biopsy.
Prostate MRI is also used for surgical planning for men undergoing robotic prostatectomy. It has also shown to help surgeons decide whether to resect or spare the neurovascular bundle, determine return to urinary continence, and help assess surgical difficulty.
For Prostate MRI exists the PI-RADS Reporting system. PI-RADS is an acronym for Prostate Imaging-Reporting and Data System, defining standards of high-quality clinical service for multi-parametric Magnetic Resonance Imaging (mpMRI), including image creation and reporting.
Biopsy Test
If cancer is suspected, a biopsy is offered expediently. During a biopsy a urologist or radiologist obtains tissue samples from the prostate via the rectum. A biopsy gun inserts and removes special hollow-core needles (usually three to six on each side of the prostate) in less than a second. Prostate biopsies are routinely done on an outpatient basis and rarely require hospitalization. Antibiotics should be used to prevent complications like fever, urinary tract infections, and sepsis even if the most appropriate course or dose of the antibiotic is still undefined.[70] Fifty-five percent of men report discomfort during prostate biopsyProstate cancer staging
An important part of evaluating prostate cancer is determining the stage, or how far the cancer has spread. Knowing the stage helps define prognosis and is useful when selecting therapies. The most common system is the four-stage TNM system (abbreviated from Tumor/Nodes/Metastases). Its components include the size of the tumor, the number of involved lymph nodes, and the presence of any other metastases.The most important distinction made by any staging system is whether or not the cancer is still confined to the prostate. In the TNM system, clinical T1 and T2 cancers are found only in the prostate, while T3 and T4 cancers have spread elsewhere. Several tests can be used to look for evidence of spread. Medical specialty professional organizations recommend against the use of PET scans, CT scans, or bone scans when a physician stages early prostate cancer with low risk for metastasis. Those tests would be appropriate in such cases as when a CT scan evaluates spread within the pelvis, a bone scan look for spread to the bones, and endorectal coil magnetic resonance imaging to closely evaluate the prostatic capsule and the seminal vesicles. Bone scans should reveal osteoblastic appearance due to increased bone density in the areas of bone metastasis—opposite to what is found in many other cancers that metastasize.
After a prostate biopsy, a pathologist looks at the samples under a microscope. If cancer is present, the pathologist reports the grade of the tumor. The grade tells how much the tumor tissue differs from normal prostate tissue and suggests how fast the tumor is likely to grow. The Gleason system is used to grade prostate tumors from 2 to 10, where a Gleason score of 10 indicates the most abnormalities. The pathologist assigns a number from 1 to 5 for the most common pattern observed under the microscope, then does the same for the second-most-common pattern. The sum of these two numbers is the Gleason score.
Prevention
Diet and lifestyleThe data on the relationship between diet and prostate cancer is poor. In light of this the rate of prostate cancer is linked to the consumption of the Western diet.There is little if any evidence to support an association between trans fat, saturated fat, and carbohydrate intake and risk of prostate cancer.Evidence regarding the role of omega-3 fatty acids in preventing prostate cancer does not suggest that they reduce the risk of prostate cancer, although additional research is needed.Vitamin supplements appear to have no effect and some may increase the risk.High calcium intake has been linked to advanced prostate cancer.[83] Consuming fish may lower prostate cancer deaths but does not appear to affect its occurrence.Some evidence supports lower rates of prostate cancer with a vegetarian diet.There is some tentative evidence for foods containing lycopene and selenium.Diets rich in cruciferous vegetables, soy, beans and other legumes may be associated with a lower risk of prostate cancer, especially more advanced cancers.
Men who get regular exercise may have a slightly lower risk, especially vigorous activity and the risk of advanced prostate cancer.
Medications
In those who are being regularly screened, 5-alpha-reductase inhibitors (finasteride and dutasteride) reduce the overall risk of being diagnosed with prostate cancer, but there are insufficient data to determine if they have an effect on the risk of death and they may increase the chance of more serious cases.Signs and symptoms
 Bladder stones are small mineral deposits that can form in the bladder. In most cases bladder stones develop when the urine becomes very concentrated or when one is dehydrated. This allows for minerals, such as calcium or magnesium salts, to crystallize and form stones. Bladder stones vary in number, size and consistency. In some cases bladder stones do not cause any symptoms and are discovered as an incidental finding on a plain radiograph. However, when symptoms do occur, these may include severe lower abdominal and back pain, difficult urination, frequent urination at night, fever, painful urination and blood in the urine. The majority of individuals who are symptomatic will complain of pain which comes in waves. The pain may also be associated with nausea, vomiting and chills.
Bladder stones are small mineral deposits that can form in the bladder. In most cases bladder stones develop when the urine becomes very concentrated or when one is dehydrated. This allows for minerals, such as calcium or magnesium salts, to crystallize and form stones. Bladder stones vary in number, size and consistency. In some cases bladder stones do not cause any symptoms and are discovered as an incidental finding on a plain radiograph. However, when symptoms do occur, these may include severe lower abdominal and back pain, difficult urination, frequent urination at night, fever, painful urination and blood in the urine. The majority of individuals who are symptomatic will complain of pain which comes in waves. The pain may also be associated with nausea, vomiting and chills.Bladder stones vary in their size, shape and texture- some are small, hard and smooth whereas others are huge, spiked and very soft. One can have one or multiple stones. Bladder stones are somewhat more common in men who have prostate enlargement. The large prostate presses on the urethra and makes it difficult to pass urine. Over time, stagnant urine collects in the bladder and minerals like calcium start to precipitate. Other individuals who develop bladder stones include those who have had spinal cord injury, paralysis, or some type of nerve damage. When nerves to the back are damaged, the bladder cannot empty, resulting in stagnant urine.
By Steven Fruitsmaak - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=4132491
Causes
Bladder stones may occur whenever the kidneys, bladder, or ureters become inflamed, which may occur when the urine becomes too concentrated or when the body becomes dehydrated. Minerals such as calcium and magnesium crystallize into the stones, which then can cause such symptoms as lower back or abdominal pain or difficulty with urination. The use of urinary catheters may cause a bladder stone. Individuals who are paralyzed or are unable to adequately pass urine may require the use of small plastic tubes (catheters) placed into the bladder. The use of these tubes may lead to an infection, which irritates the bladder, resulting in stone formation. Finally, a kidney stone may travel down the ureter into the bladder and become a bladder stone. There is some evidence indicating that chronic irritation of the bladder by retained stones may increase the chance of bladder cancer. Urinary schistosomiasis, a disease caused by the digenean trematode Schistosoma haematobium, has been implicated in the development of vesical calculi. However, evidence accumulated thus far has not supported this hypothesis.Urinary stones may be composed of the following substances:
- Calcium oxalate monohydrate (whewellite)
- Calcium oxalate dihydrate (weddellite)
- Calcium phosphate
- Magnesium phosphate
- Ammonium phosphate
- Ammonium magnesium phosphate (struvite)
- Calcium hydroxyphosphate (apatite)
- Uric acid and its salts (urates)
- Cystine
- Xanthine
- Indigotin (rare)
- Urostealith (rare)
- Sulfonamide (rare)
Prevention
The best way to prevent bladder stones is to drink plenty of liquids. Juices containing citrates are thought to reduce the risk of stone formation. A study published in the Clinical Journal of the American Society of Nephrology indicate orange juice is more effective at preventing stone formation than other citrus juices. Men who have difficulty with urination due to prostatic hypertrophy should seek treatment. In those with benign prostatic hyperplasia urinating in a sitting position appears to improve bladder emptying which might decrease bladder stones in this group.Management
Increasing fluid intake can facilitate the passage of small bladder stones. However, larger stones may require other methods of treatment.Fragmentation of bladder stones can be achieved by use of a cystoscope which is inserted into the bladder. The urologist visualizes the stone and uses ultrasonic energy or laser lithotripsy to cause fragmentation of the stones into small pieces, which are then flushed out of the bladder. This procedure requires anesthesia and may require admission to a hospital. Complications of this treatment include infection and damage to the bladder.Some stones are too large even for cystoscopic treatment and may require open cystotomy, in which an incision is made in the bladder and the stones are removed manually.Source : Wikipedia










